Peritoneal Endometriosis
Dr. Abhishek Mangeshikar & Ms. Sagaya Kirti
The peritoneum is a thin membrane lining the abdominal cavity. Genetic or hereditary conditions predispose it to room endometriotic implants that cause pain. Peritoneal type of pain may vary in severity but a majority of patients report severe pain with a very particular peritoneal quality.
Peritoneal endometriosis is the most difficult type of endometriosis to diagnose because it may not show up on imaging and is only diagnosed on laparoscopy. Furthermore because of the varied appearance of peritoneal endometriosis, it may be missed at laparoscopy by untrained or inexperienced surgeons.
There are various presentations of peritoneal endometriosis:
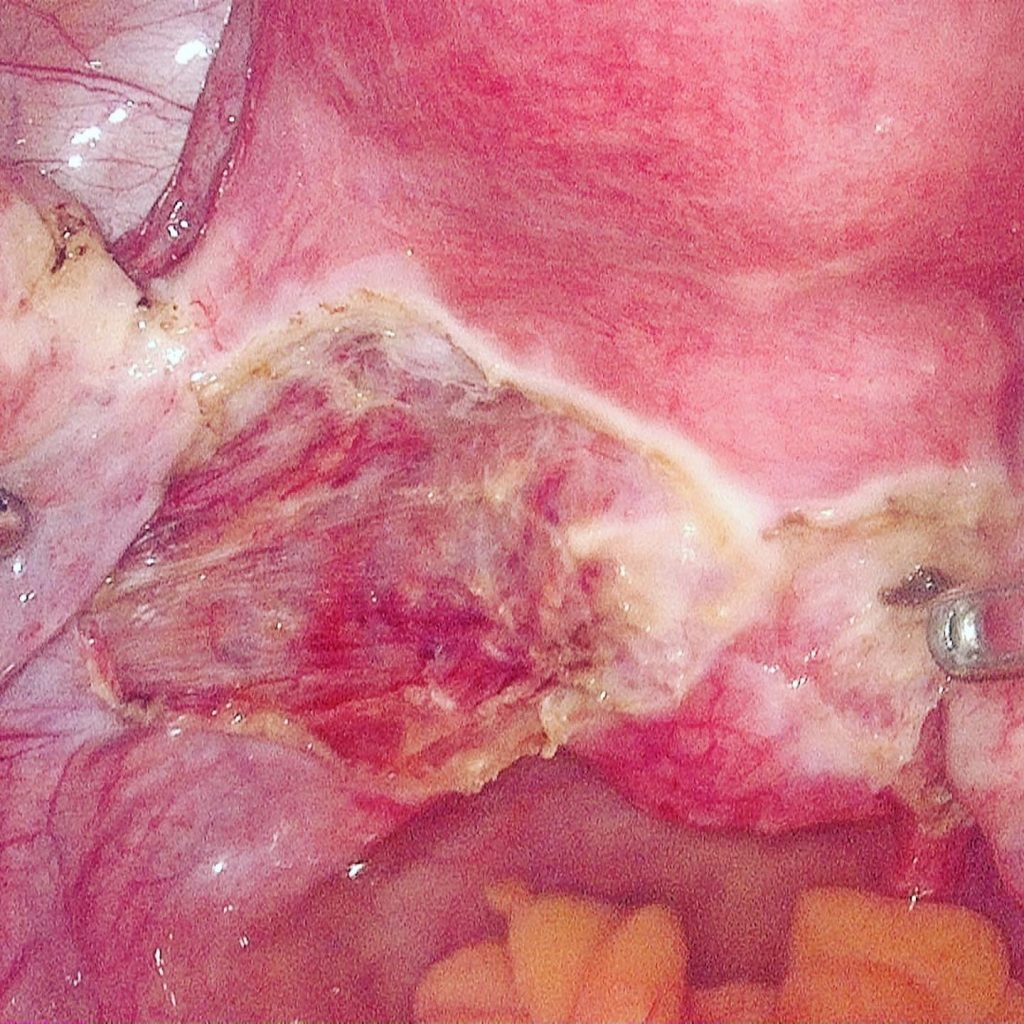
1: Classical bluish- black lesions: These are the typical lesions described in most textbooks about endometriosis and are the easiest to identify. When they are fulgurated they turn brown (Semm’s thermocolour test).
On closer inspection one can notice the subtler lesions extending all the way across toward the right
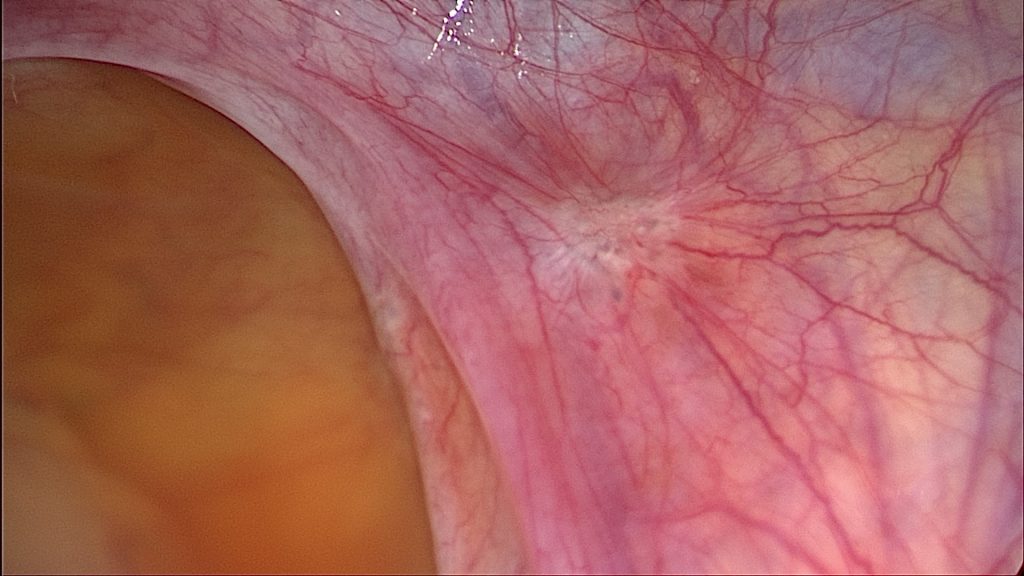
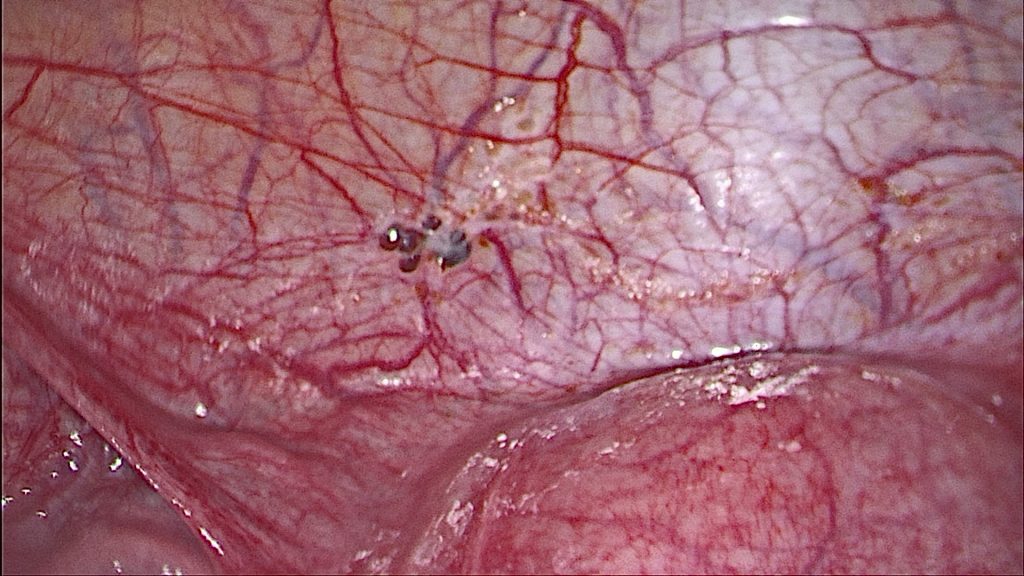
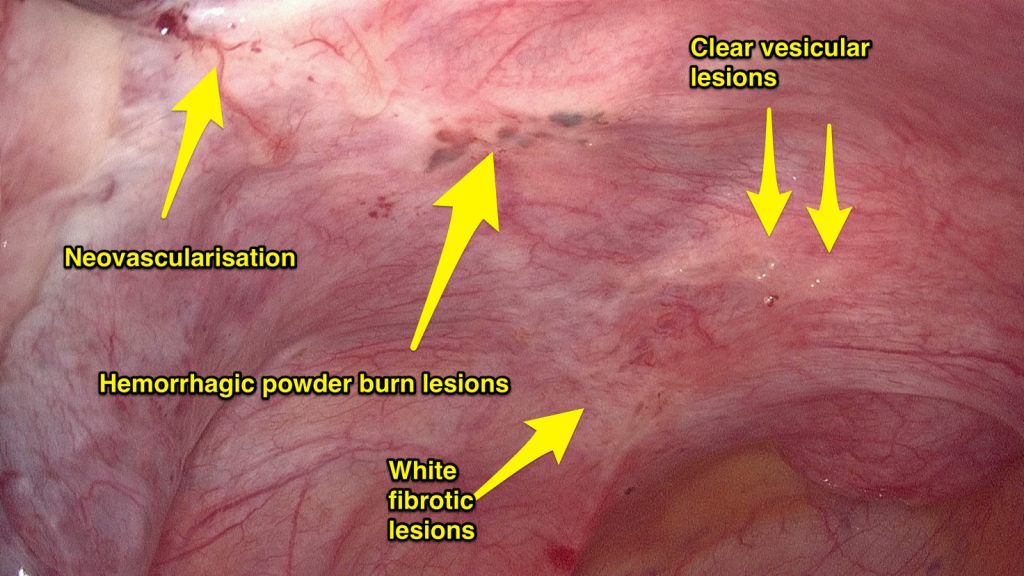
2: Atypical subtle lesions: These may vary in appearance and can sometimes only be identified by “near contact laparoscopy” which is by bringing the laparoscope upto 2cms away from the tissue to be able to appreciate the subtle changes in the peritoneal tissue. These may vary from colourless small cystic blebs, to yellowish fluid filled ones. There may be angry looking capillaries coalescing over an area (suggestive of neoangiogenesis) or white scarified opacities overlying these vessels (due to tissue injury and repair).
Unfortunately these lesions are morphologically more active than the classical lesions and are more likely to be missed by routine gynecologists not trained in identification of the atypical appearances. They may be responsible for severe peritoneal quality pain that many women have complained of and ended up with negative laparoscopies solely because these lesions were missed.
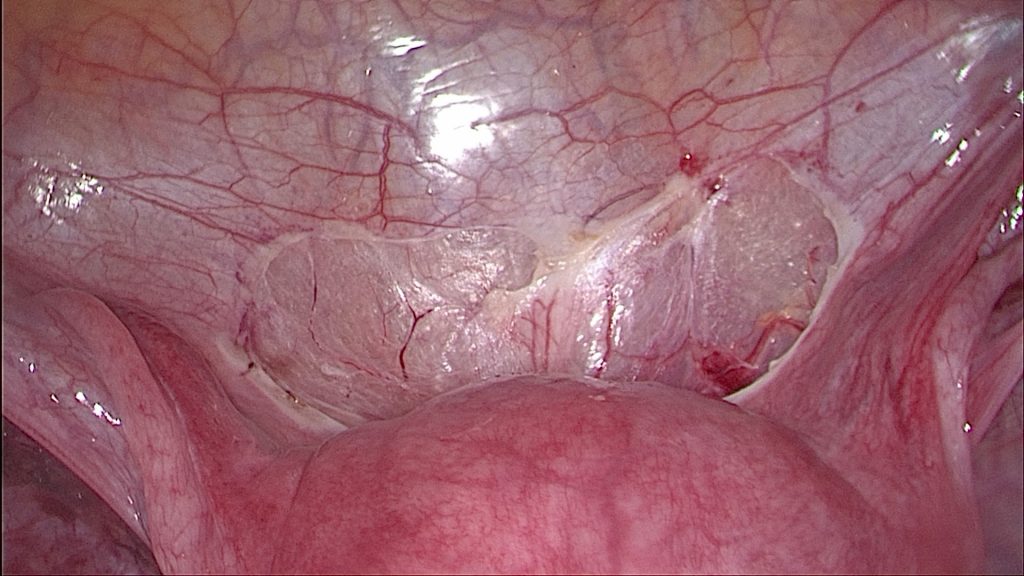
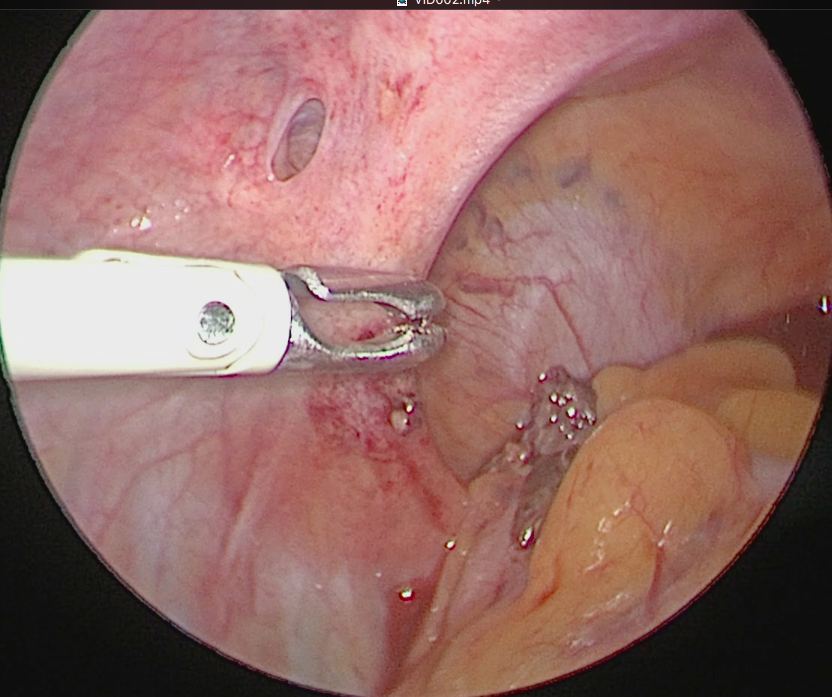
3: Peritoneal pockets or Allen Masters syndrome: These are defects or windows in the peritoneum which harbor endometriosis deep within and are also often overlooked as congenital defects within the peritoneum. It is imperative to turn the pocket inside out and excise the entire defect to ensure complete excision.
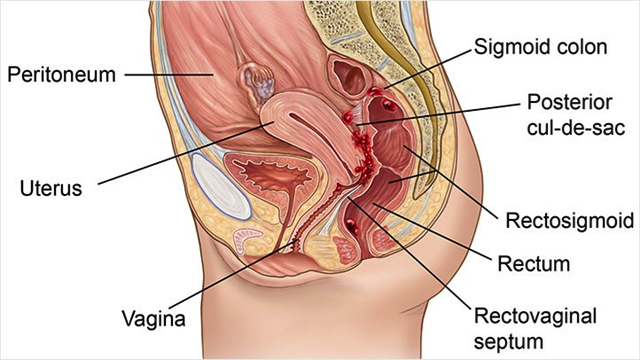
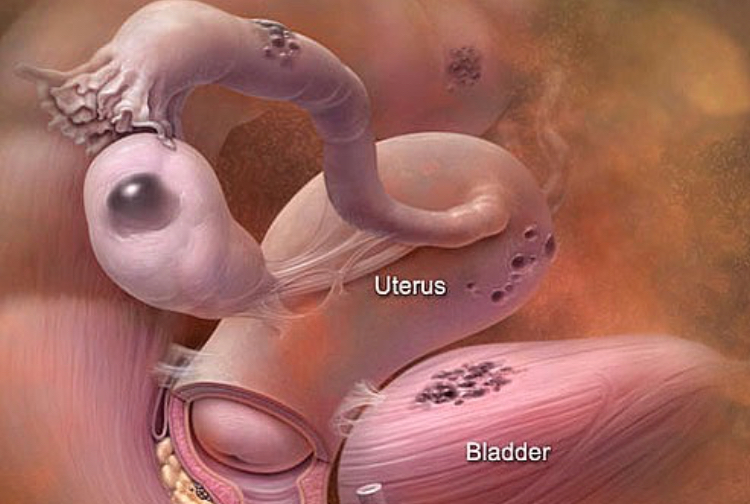
Possible locations where implants can be found.
Peritoneal disease can be found anywhere in the abdomen or pelvis that is covered by peritoneum, i.e., almost every organ and/or surface in the abdomen or pelvis.
The more common places where peritoneal endometriosis is often seen but not limited to are:
- Psoas muscle
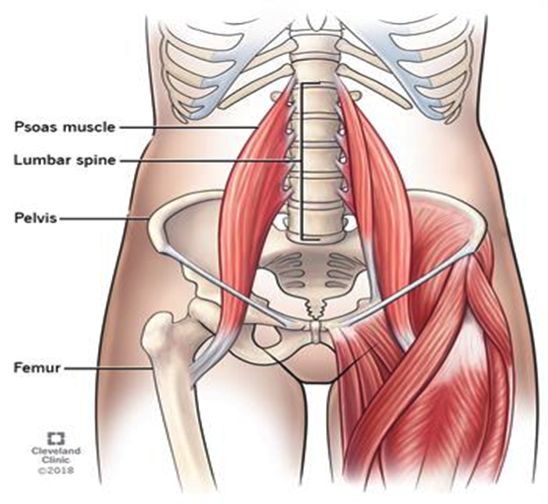
- Area under ovaries (superior part of ovarian fossa)
- Periureteral ovarian fossa (where ovaries rest)
- Pelvic brim
- Uterosacral ligaments
- Cul-de-sac.
- Rectal mesentry
- Sigmoid mesentry
Progression of the disease.
At initial stages, the implants just adhere to surfaces of the peritoneum without invading the underlying tissue and stroma. Since the implants are hormone responsive, i.e., they are responsive predominantly to estrogen, they grow over time. Now, the endometriotic implants- considered foreign by our natural immune system- are fought against and seldom is the battle won. This results in increased cytokines or immune factors within the peritoneal cavity. These cytokines sensitize the peripheral nerves and stimulate a sensation of pain . They cause a characteristic intense pain or “peritoneal quality pain” which may be more severe than those with advanced stage disease.
When left untreated the endometriotic implants develop adhesions in the ovary causing chocolate cysts or ovarian endometriosis and/or penetrate deep (>5mm) into the tissues causing deep infiltrating endometriosis (DIE) both of which are categorized as separate type and are explained in detail separately.
Complications associated with superficial peritoneal endometriosis.
- Chronic pelvic pain.
- Dysmenorrhea.
- Painful bowel movements if implants are present in the rectum.
- Dyspareunia if implants are present in the cul-de-sac or in rectovaginal septum or in the retrocervical area.